Definition
An inflammation of the meninges, especially the arachnoid mater and the pia mater, often secondary to infection. Edema and inflammatory infiltrates lead to fever, focal neurological deficits, decreased level of consciousness, and seizure.
- Infectious causes can be bacterial, viral, fungal, or parasitic
- While the etiology is usually infectious, ultimately it is the inflammatory changes in the CNS that cause morbidity and mortality
Etiology
Lancet 2003; 361: 2139–48.
Curr Opin Infect Dis 2007; 20(3):272-277.
Causative organisms vary by age group:
|
Neonates (<3 mo) |
Children |
Adults |
Elderly (>65) |
|
Group B Streptococcus
Escherichia coli
Listeria monocytogenes |
Streptococcus pneumoniae (pneumococcus)
Neisseria meningitidis (meningococcus)
Haemophilus influenzae type B (less common now with the advent of the HiB vaccination) |
Streptococcus pneumoniae
Neisseria meningitidis
(these two organisms cause 80% of cases) |
Streptococcus pneumoniae
Neisseria meningitidis
Listeria monocytogenes |
If no organism can be isolated with routine culture and sensitivity assays of cerebrospinal fluid (CSF), the condition is called aseptic meningitis, and the etiology is likely viral (e.g. Enterovirus, HIV and HSV). Less common etiologies for aseptic meningitis include tuberculous meningitis (Mycobacterium tuberculosis), Lyme disease (Borrelia spp.), parasitic infections (e.g. Taenia solium, Toxoplasma gondii), and malignancy.
Pathogenesis
Ther Adv Neurol Disord. 2009; 2(6):401-412.
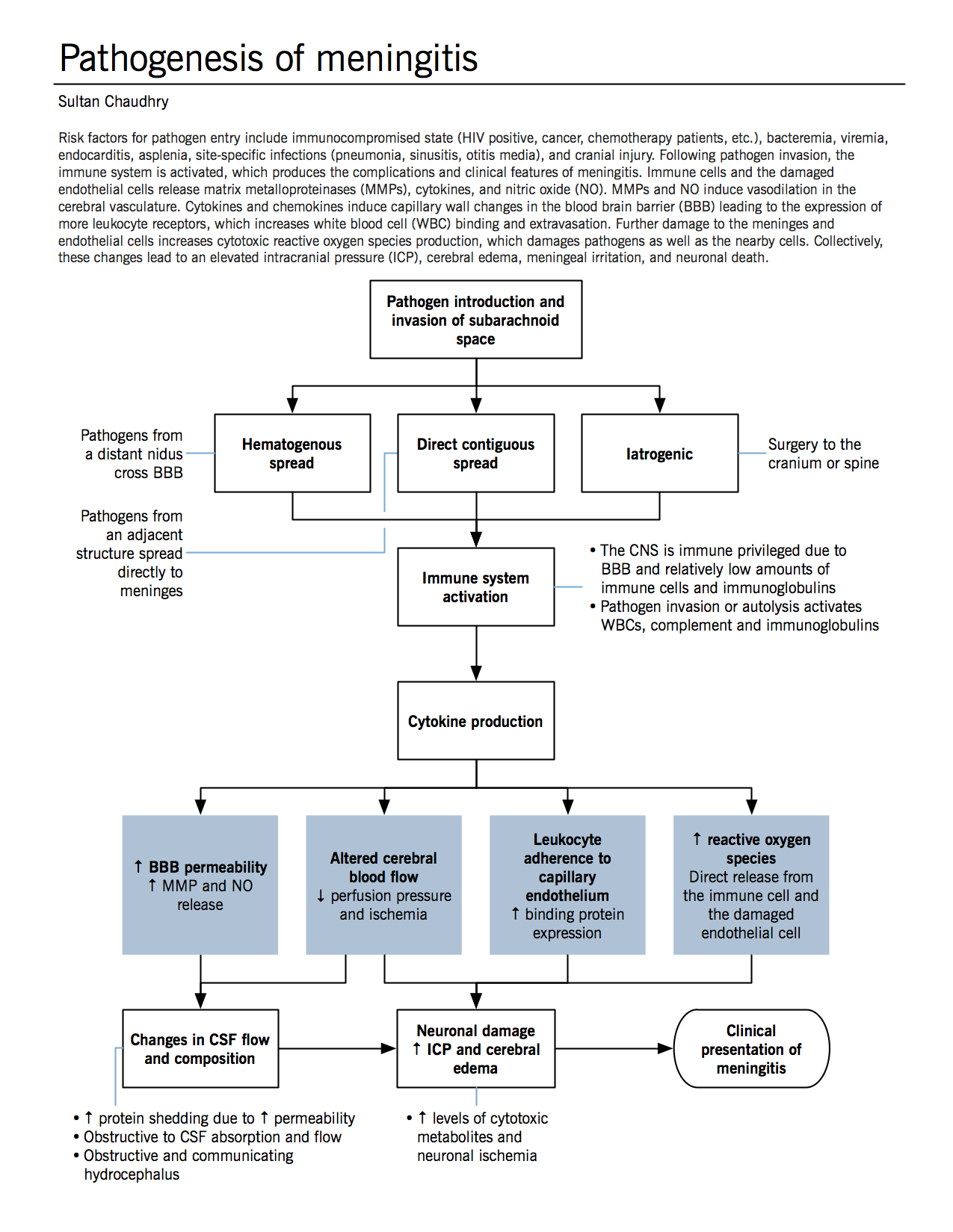
See figure.
Clinical features and pathophysiology
JAMA. 1999 Jul 14;282(2):175-81.
N Engl J Med 2004; 351:1849-1859.
Pediatrics. 2010 Nov;126(5):952-60.
|
Symptom |
Sign |
Mechanism |
|
Chills, rigors |
Fever (T>38°) |
Endogenous cytokines (released during the immune response to the invading pathogens) affect the thermoregulatory neurons of the hypothalamus, changing the central regulation of body temperature.
Invading viruses or bacteria produce exogenous substances (pyrogens) that can also re-set the hypothalamic thermal set point. |
|
Nuchal rigidity (neck stiffness) |
Brudzinski sign and Kernig sign |
Flexion of the spine leads to stretching of the meninges.
In meningitis, traction on the inflamed meninges is painful, resulting in limited range of motion through the spine (especially in the cervical spine). |
|
Altered mental status |
Decreased Glasgow Coma Scale (GCS) |
↑ ICP → brain herniation → damage to the reticular formation (structure in the brainstem that governs consciousness) |
|
Focal neurological deficits, e.g. vision loss |
Examples: cranial nerve palsies, hemiparesis, hypertonia, nystagmus |
Cytotoxic edema and ↑ ICP lead to neuronal damage.
Signs or symptoms depend on the affected area (cerebrum, cerebellum, brainstem, etc.) |
|
Seizures |
|
Inflammation in the brain alters membrane permeability, lowering the seizure threshold. Exact seizure pathophysiology is unknown. |
|
Headache |
Jolt accentuation of headache: headache worse when patient vigorously shakes head |
Bacterial exotoxins, cytokines, and ↑ ICP stimulate nociceptors in the meninges (cerebral tissue itself lacks nerve endings that generate pain sensation). |
|
Photophobia |
|
Due to meningeal irritation. Mechanisms unclear; pathways are thought to involve the trigeminal nerve. |
|
Nausea and vomiting |
|
↑ ICP stimulates the area postrema (vomiting centre), causing nausea and vomiting. |
|
|
Petechial rash |
Meningococcemia (due to N. meningitidis) |
In the pediatric population, all of the above signs and symptoms are applicable. Additional signs and symptoms in children include:
- Bulging fontanelles
- Bones of the skull do not join fully (form sutures) until age 2
- ↑ ICP → meninges protrude through gaps in skull bones
- Jaundice
- Impaired bilirubin excretion
- Exact mechanism unclear, associated with sepsis
- Reduced feeds, irritability, lethargy, and toxic appearance
- Fever, shock and cerebral edema can lead to such manifestations in children
Treatment
Clin Infect Dis. (2004) 39 (9):1267-1284.
The goal of treatment is to maintain cerebral perfusion pressure by preserving the mean arterial pressure (e.g. fluid resuscitation) and normalizing intracranial pressure (e.g. elevating the head, hyperventilation, controlling seizure activity; hyperventilation causes hypocapnia-mediated cerebral vasoconstriction).
Cerebral perfusion pressure = Mean arterial pressure – ICP
The mainstay of treatment for bacterial meningitis is antibiotics; choice of antibiotic depends on the organism isolated from blood and CNS cultures. Any delay in treatment results in increased morbidity and mortality, so antibiotics are often started empirically based on the age of the patient (see table in Etiology above) and any risk factors they may have (e.g. if they are immunocompromised or have recently had neurosurgery). The antibiotic regimen is then adjusted once the causative organism is known. Corticosteroids can be used adjunctively to reduce inflammation in the brain if the pathogen is Streptococcus pneumoniae.
In viral meningitis, the treatment is supportive. In patients with suspected Herpes Simplex Virus (HSV) infection, empiric antiviral therapy is started to prevent complications of HSV encephalitis.
Distinguishing between viral and bacterial meningitis is done using blood and CSF cultures, as well as lumbar puncture opening pressure (which reflects ICP) and CSF analysis.
|
|
Bacterial meningitis |
Viral meningitis |
Mechanism |
|
Opening pressure (N: 8-20 cm H2O) |
Elevated (20-30 cm H2O) |
Normal or mildly increased |
Increased inflammation in bacterial meningitis results a higher ICP and thus a high opening pressure. |
|
CSF glucose (N: 2.8-4.4 mmol/L; blood:CSF glucose ratio is normally 0.3-0.9) |
Decreased (<2.2 mmol/L) |
Normal |
In bacterial meningitis, glucose transport from the blood into the CSF is impaired; inflammation of the meninges leads to decreased glucose receptor expression. There is also increased anaerobic glycolysis by leukocytes and brain cells. |
|
CSF protein (N: 0.15-0.45 g/L) |
Very high >1.5 g/L |
Mildly increased 0.5-2 g/L |
Bacterial meningitis leads to a more permeable blood brain barrier (due to increased inflammation). Protein leaks into the subarachnoid space from the blood, resulting in markedly increased CSF protein levels. |
Surgical management is indicated where there is extremely increased intracranial pressure, infection of an adjacent bony structure (e.g. mastoiditis), skull fracture, or abscess formation.